|
Techniques and Technical Tips for Success |
|
The STARR
procedure for Obstructed Defecation |
|
Alfonso Carriero,
M.D.
Director, Pelvic
Floor Center
Montecchio
Emilia Hospital
Reggio Emilia (Italy)
tel.
: 0522.860.407 - 0522.860.298
Fax : 0522.860.292
e-mail :
info@acarriero.it
website :
www.acarriero.it |
|
Objectives: |
-
Identify the anatomical and functional
lesions associated with clinical
symptoms and signs of obstructed
defecation
-
Selective criteria
-
Technical steps and tips
|
|
INTRODUCTION |
|
Obstructed defecation is a common complaint
referred to coloproctologists and may be
associated with rectocele and/or rectoanal
intussusception . The patient (usually a
female) experiences a sense of incomplete
evacuation and often defecates only with the
use of perineal support, or insertion of
fingers into the vagina and/or the anal
canal. Laxative or enema abuse is frequent,
and can become less effective with time.
Various surgical techniques, with a
transanal, transperineal, transvaginal,
transabdominal or double abdomino-vaginal
approach have been proposed for the
treatment of this condition, however there
is little agreement on best approach for
dealing with the problem.
Coloproctologists usually prefer transanal
techniques, that allow correction of
frequently associated disorders of the anal
canal. At present no trial has clearly
established whether a transanal approach is
better than other alternatives and there are
no data to show which transanal technique is
best. A new technique, employing a circular
stapler , combined with a perineal
levatorplasty, has been recently proposed to
correct internal rectal mucosal prolapse and
rectocele . However perineal levatorplasty
may result in delayed healing of the
perineal wound and later dyspareunia . To
overcome this, Longo recently proposed the
use of a double circular stapler, that
reduces the cul the sac of the rectocele and
in addition corrects the rectal
intussusception. |
|
SELECTIVE CRITERIA |
|
The
inclusion criteria
for surgical treatment with stapled
trans-anal rectal resection were
clinical, radiological, manometric,
sonographic: |
|
Clinical criteria:
|
-
Incomplete, prolonged, and difficult
evacuation with constant use of enemas
-
Use/abuse of laxatives
-
Rectal and/or vaginal digitations to
facilitate rectal emptying
-
CCF constipation score > 15
-
Rectal or vaginal symptoms present for
longer than 12 months
-
Failure of medical (2 litres/day of water,
high-fiber diet, lactulose 10 g/day
-
Failure of rehabilitative treatment (bimodal
rehabilitation).
|
|
Radiological criteria |
|
a) Defecography
-
Recto-anal intussusception with enfolding ≥
10 mm
-
Rectocele deeper than 3 cm on straining
-
Inability to achieve complete evacuation of
barium paste despite a measurable
increase in the anorectal angle between rest
and attempted defecation
b) Colonic Transit Time
|
|
Functional criteria |
|
a) Computerized anorectal manometry
|
|
Morphological criteria
|
|
a) Anal
ultrasound
These
clinical symptoms and radiological signs must be present
contemporaneally as
selection criteria for
surgery:
-
Failure
of medical therapy (1.5 litres./day of water, high-fiber diet,
lactulose 10 g/day)
-
Sense of
incomplete evacuation and straining
-
Defecation with use of perineal support
-
Self-digitation
into the vagina, or anus
-
Evacuation obtained only with enemas
-
Rectocele deeper than 3 cm at defecography on straining
-
Reteined
barium contrast after defecation
-
Recto-anal infolding > 3 mm.
|
|
At least
2 clinical + 2 radiological parameter had to be present.The presence
of
concomitant anal disease (e.g.haemorrhoids, anal fissure) was not a
contraindication to the
operation. |
|
All
patients must give informed written consent. All surgical teams had
previous
experience in surgical treatment of rectocele and use of stapler in
the treatment of
haemorrhoidal prolapse (at least 30 operations). |
|
We
suggest the use of CCF Costipation and Continence Score Index and
SF36- GIQLI , to have a
more precise measure of constipation, faecal incontinence and
quality of life. |
|
Some
exclusion criteria were applied. The following patients are usually exluded for:
-
Paradoxical pubo-rectalis
-
Previous
pelvic or anorectal surgery
-
IBD and
IBS
-
Neurologic diseases
-
Psychiatric illness
-
Total or
partial faecal incontinence
-
Diabetes
-
Systemic
sclerosis
|
|
SURGICAL TECHNIQUE |
|
|
|
Bowel
preparation |
|
Preoperatively, a cleansing enema is given, and the patient received
a routine antibiotic
prophylaxis (cefotaxime 2 g and metronidazole 500 mg i.v.),
immediately after the
induction of anaesthesia. |
|
Anaesthesia |
|
The
operation was performed under general, caudal , or loco-regional
anaesthesia,
|
|
Position
|
|
It’s
mandatory that the patient is in lithotomy position to check
completely, in the same time the
vagina and the anal sphincters. |
|
Theatre
Preparations
|
|
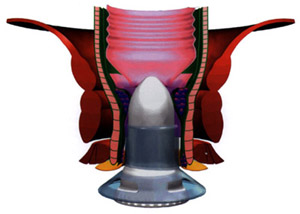
It’s
need 2 PPH01(Ethicon-Endosurgery, Inc, Cincinnati,Ohio sets
containing: a circular stapler,
a disposable circular anal dilator with obturator, and a windowed
anoscope and than a
metallic spatula and suture threader. |
|
The
suture material is : 2-0 Prolene
75 cm for purse-string sutures, 3-0 Vicryl
for suture ligature
of blood vessels and 1-0 Ethibond
for fixation of Anal Dilator. |
|
SURGICAL STEPS |
|
|
|
Placing
of the Anal Dilator |
|
After
gentle dilation of the anal verge, I suggest to insert a gauze swab
to slightly stretch the anal
canal and the anal dilator was introduced now and fixed by 4
stitches to the anal skin.
Relax the anal sphinctermuscle by repeated insertion of the
lubricated obturator. |
 |
 |
|
Determing the prolapse degree |
|
Pull
back the previously inserted gauze swab together with the prolapsed
rectum through the anal
dilator. If the pulled-out rectal wall protrudes more than half-way
out of anal
dilatator, this indicates a pronunced prolapse, making it advisable
to carry out 3-4 purse string
sutures along the anterior rectal wall; if the prolapse is less
pronounced, two sutures will be
sufficient. |
|
Inserting the Spatula and the Anoscope
|
|
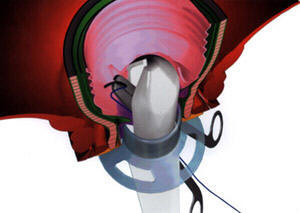 Through
the posterior window of anal dilator, we insert a metallic spatula
for about 8 –10 cm. into the rectum to protect the posterior rectal wall when the circular
stapler is fired.
We
suggest
the use of fingers into the rectum to move the prolapsing rectal
wall, thus avoiding injury
or a perforation of the rectum. Now we
apply the anoscope into the anal dilator, to protect the opposite
rectal wall, so that the
opening of the anoscope initially points at west direction (9.00
o’clock). Through
the posterior window of anal dilator, we insert a metallic spatula
for about 8 –10 cm. into the rectum to protect the posterior rectal wall when the circular
stapler is fired.
We
suggest
the use of fingers into the rectum to move the prolapsing rectal
wall, thus avoiding injury
or a perforation of the rectum. Now we
apply the anoscope into the anal dilator, to protect the opposite
rectal wall, so that the
opening of the anoscope initially points at west direction (9.00
o’clock). |
|
Carrying
out the Purse-string suture |
|
Three
half purse-strings with Prolene Tm 2-0
(Ethicon,Somerville,NJ,USA) are inserted above
the dentate line, 1-2 cm apart , to include the top of rectocele. We
place the first
semicircular purse-string 2 – 3 cm. above the base of the
haemorrhoidal tissue, from west to east
direction, turning the anoscope accordingly.
The
second transverse suture should be carried out approximately 2 – 2.5
cm above the first purse-string. The last suture is placed 2 – 2.5 cm above. We knot
the suture ends at west and
east to ensure even traction of the prolapse later on. |
|
Inserting the Circular Stapler |
|
We pull
the ends of the two threads in the direction of 12.00 o’clock,
making sufficient space
for the insertion of circular stapler. The stapler must be insert
completely open and the head
of the device is positioned right above the semicircular
purse-strings. Following that, we
use the suture-threader to pull out the ends of the threads through
the lateral holes of casing. |
|
Firing
the Circular Stapler |
|
Now we
close slowly the stapler down to 2 cm, making sure that its head
remain
positioned above the semicircular purse-string sutures. We apply a
moderate traction of
pursestring, gently push the stapler further into the rectum until
the casing is inserted 4 cm into
anal dilator; exerting further traction onto the sutures, tighten
the stapler until it is almost
completely closed. |
|
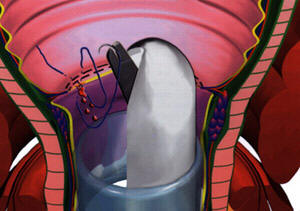
In
female patients, we insert two fingers into the vagina and by
pushing against the anterior
rectal wall make sure that the top of the stapler casing is above
the levator ani muscle,
the prolapse has been drawn into the casing and the posterior
vaginal wall is freely
movable and not caught in the stapler. |
|
Afterwards, we close the stapler completely and
check by means of the display scale; to achieve optimum closure, the
markings must be at
lower end of the scale. Now, it’s possible to fire in axial position
to the rectum; than we open
the stapler by giving it an one-quarter or half turn, at the least
we remove
carefully. |
|
Checking
of the Anastomosis
|
|
Quite
frequently firing the circular stapler will cause the “mucous
bridge” at the posterior side,
right above the metallic spatula,in that case we use scissors to
separate the
structure. After we examine the anastomosis with a gauze swab. The anterior
stapled line was
renforced using 2-3 Vicryl Tm 3-0 sutures
(Ethicon) and inspected for bleeding. |
|
Furthermore, we carefully examine the resected tissue to determine that the rectal wall has been
removed completely. |
|
Inserting the Spatula and the Anoscope (for the resection of
posterior rectal wall) |
|
Through
the anterior window of anal dilator, we reposite the samemetallic
spatula for about 8 –10
cm. into the rectum to protect now the anterior rectal wall and the
anterior
anastomosis, when the circular stapler is fired. We suggest the use
of fingers into the rectum
to feel the rectal anastomosis, thus avoiding an injury. |
|
Now we
apply the anoscope into the anal dilator, to protect the opposite
rectal wall, so that the
opening of the anoscope initially points at east direction (3.00
o’clock). |
|
Carrying
out the Purse-string suture (for the resection of posterior rectal
wall) |
|
The
procedure was repeated in the posterior rectal wall .Two or three
half purse-strings with
Prolene Tm 2-0 were prepared above the dentate
line, to reduce the posterior rectal
intussusception. We place the first semicircular purse-string 2 – 3
cm. above the base of the
haemorrhoidal tissue, from east to west direction. |
|
With the
first anastomosis, we create two folds (“dog ears”), in right and
left rectum. We
suggest to start, in this time, with the first purse-string under
the base of left fold until the
right side. The second transverse suture should be carried out above
the folds, and more
laterally; in that way, we achieve the redundat prolapse into the
casing. If ii’s necessary, another
suture is placed 2 – 2.5 cm above. |
|
Inserting the Circular Stapler and Firing the Circular Stapler
(for
the resection of posterior rectal wall) |
|
We pull
the ends of the two threads in the direction of 12.00 o’clock,
making sufficient space
for the insertion of circular stapler. The stapler must be insert
completely open and the head
of the device is positioned right above the semicircular
purse-strings. Following that, we
use the suture-threader to pull out the ends of the threads through
the lateral holes of
casing. Now we close slowly the stapler down to 2 cm, making sure
that its head remain positioned above the semicircular purse-string
sutures. |
|
We apply a
constant traction
of pursestrings and insert the stapler-casing into the rectum until
a resistance caused
by the anterior anastomosis. Afterwards, we close the stapler
completely and check by
means of the display scale. Fire in axial position to the rectum;
than we open the stapler
by giving it an one-quarter or half turn, at the least we remove
carefully. |
|
Checking
of the Anastomosis |
|
Also now
frequently firing the circular stapler will cause the “mucous
bridge” at the anterior side,
right above the metallic spatula,in that case we use scissors to
separate the structure. |
|
After we examine the anastomosis with a gauze swab. The
posterior stapled line is
checked for bleeding using 2-3 Vicryl Tm 3-0
sutures (Ethicon).
In
particular, we suggest to fill the anal canal with saline soluction.
Through this even the
slightest bleedings can be made visible (bloodsmear formation). We
repeat this test by turning
the anoscope making sure the entire anterior anastomosis is free of
bleeding. All removed
tissues were measured and histologically examined. |
|
Finishing the operation |
|
At the
least, we consider the possibility to verify the disostruction of
rectal ampulla. We repeat
the initial prolapse test using the sponge forceps, inserting and
then pulling gauze swab. |
|
This time, it should not be possible to luxate a prolapse through
the anal dilator. Usually,
we prefer to insert a lubrificated tamponade with guiding thread
into the rectum. This is
placed directly on and above the anastomosis. The tamponade will
either act as compress
or drain for any secondary bleedings that may occur; this is removed
after 3 – 4 hours.
Now, we remove also the anal dilator. |
|
 |
|
References
-
Longo
A.: Obstracted defecation because of rectal patologies. Novel
surgical
treatment: stapled transanal rectal resection (STARR) – Syllabus 15
° AnnualColorectal Disease Symposium, February 12-14,2004
-
Boccasanta
P., Carriero A., Stuto A., Caviglia A. Stapled rectal resection for
obstructed defecation. A prospective multicenter trial.
Dis Colon Rectum 2004; 47:
1285-1297
|
 |
|
|